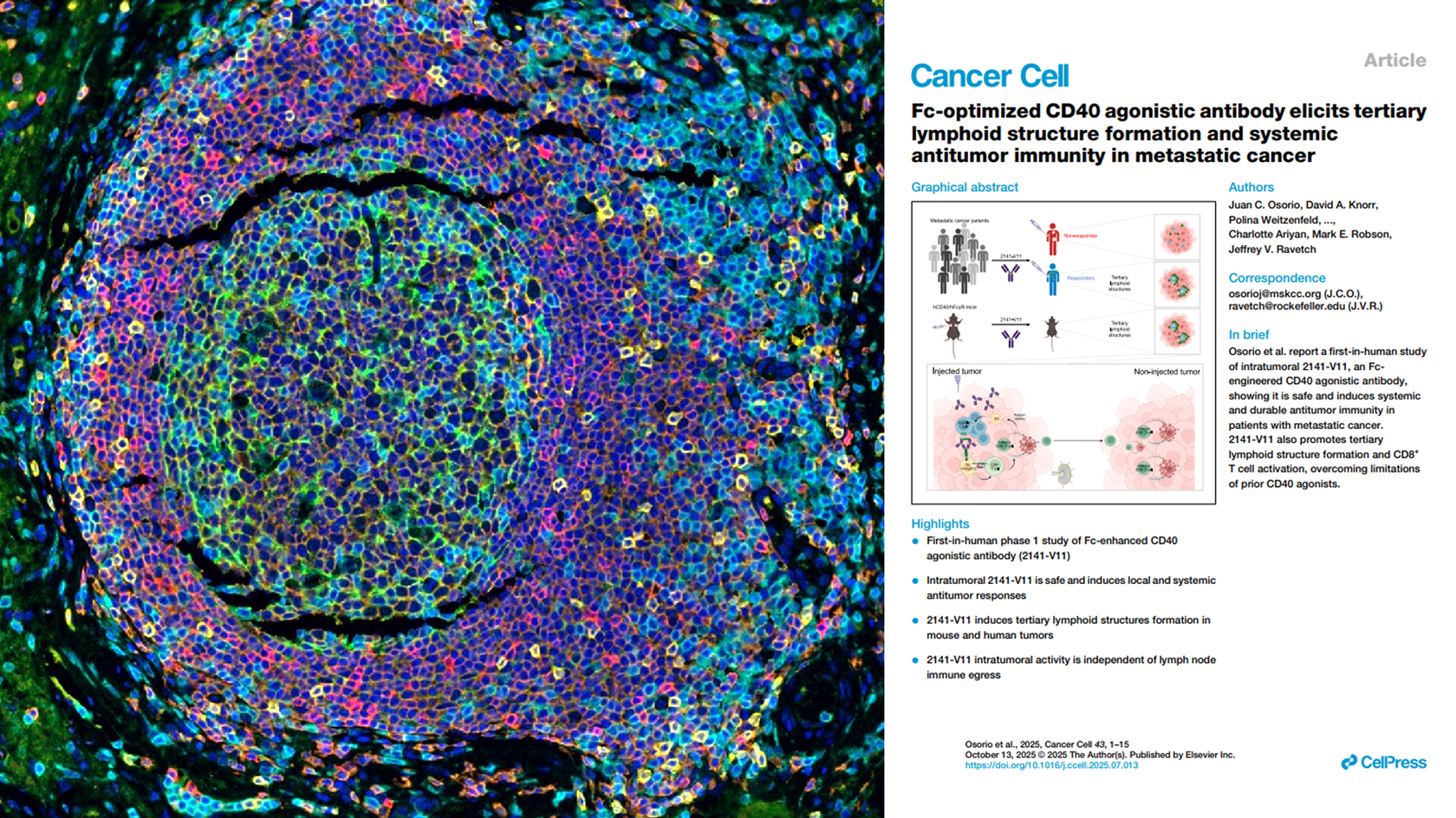
New paper out in Cancer Cell ! This collaboration with the Memorial Sloan Kettering Cancer Center (MSKCC), led by David Knorr and colleagues, shows that an Fc-optimized CD40 agonist (2141-V11), delivered intratumorally, can induce tertiary lymphoid structures (TLS) and drive systemic antitumor immunity—with complete responses reported in melanoma and breast cancer.
Beyond the headline result, these findings reinforce a key idea: TLS can be pursued as a therapeutic objective—with the right engineering and delivery, CD40 agonism can reprogram the tumor microenvironment into a self-sustaining immune ecosystem.
Explicyte supported this work with multiplex IHF staining, enabling direct visualization of TLS formation in tumor tissue. This study highlights how our translational research platform helps partners measure and interpret the impact of new immunomodulatory agents—from TLS induction and maturation to dendritic-cell activation, HEV density, and chemokine programs—leveraging spatial biology + multiplex IHF with integrated analytics.
Beyond the headline result, these findings reinforce a key idea: TLS can be pursued as a therapeutic objective—with the right engineering and delivery, CD40 agonism can reprogram the tumor microenvironment into a self-sustaining immune ecosystem.
Explicyte supported this work with multiplex IHF staining, enabling direct visualization of TLS formation in tumor tissue. This study highlights how our translational research platform helps partners measure and interpret the impact of new immunomodulatory agents—from TLS induction and maturation to dendritic-cell activation, HEV density, and chemokine programs—leveraging spatial biology + multiplex IHF with integrated analytics.
Explore our translational research platform
Soft-tissue sarcomas (STS) usually resist immune-checkpoint blockade because their micro-environment is both poorly immunogenic and actively immunosuppressive. To convert these “cold” into “hotter,” immune-responsive tumors, the phase II REGOMMUNE trial —led by Prof. Antoine Italiano at Institut Bergonié and Gustave Roussy—combined the multi-kinase anti-angiogenic agent regorafenib with the anti-PD-L1 antibody avelumab.
Between 2019 and 2021, 50 patients with advanced STS lacking mature tertiary lymphoid structures (TLS) were enrolled to test whether this strategy could boost immune-cell infiltration and improve anti-tumour activity.
Associated to this study through the RHU CONDOR, Explicyte profiled paired plasma samples (baseline → Cycle 2 Day 1) from 32 STS patients receiving regorafenib + avelumab with the Olink Explore HT panel (5300 proteins):
Explicyte ran multiplex immunofluorescence on paired biopsies from seven STS patients (pre- vs. Cycle 2 Day 1), corroborating the plasma data but also exposing barriers to efficacy:
Read the full paper
Between 2019 and 2021, 50 patients with advanced STS lacking mature tertiary lymphoid structures (TLS) were enrolled to test whether this strategy could boost immune-cell infiltration and improve anti-tumour activity.
Key findings published in Signal Transduction & Targeted Therapy
Modest efficacy, manageable safety
- Efficacy: Of the 43 TLS-negative patients who were assessable, the objective response rate was 11.4 % (all partial responses), whereas 50 % progressed on treatment. Median progression-free survival was 1.8 months.
- Safety: Forty-nine patients received at least one dose of either regorafenib or avelumab and were included in the safety analysis. Toxicities were generally low-grade and controllable; importantly, no treatment-related deaths occurred, indicating that the combination is well tolerated.
Plasma proteomics: stronger immune signals but red flags for checkpoint resistance
Associated to this study through the RHU CONDOR, Explicyte profiled paired plasma samples (baseline → Cycle 2 Day 1) from 32 STS patients receiving regorafenib + avelumab with the Olink Explore HT panel (5300 proteins):
- Immune-cell influx: Gene-ontology analysis of up-regulated proteins showed marked enrichment of CD8⁺ T-cell and B-cell signatures.
- Soluble PD-L1 surge: Soluble PD-L1 (CD274) —a known negative predictor of response to PD-(L)1 blockade—was the most strongly up-regulated protein.
- Tryptophan depletion: complementary metabolomics showed a pronounced drop in circulating L-tryptophan, a metabolic hallmark of immune activation.
Digital pathology: deeper—yet still not optimal—immune engagement
Explicyte ran multiplex immunofluorescence on paired biopsies from seven STS patients (pre- vs. Cycle 2 Day 1), corroborating the plasma data but also exposing barriers to efficacy:
- More lymphocytes: Intratumoral CD8⁺ T-cell and CD20⁺ B-cell densities rose in respectively 6 and 4 patients, yet progressive disease occurred in patients with the highest increases in CD8+ T and B cell density, showing that infiltration alone is insufficient to trigger clinical benefit.
- No TLS formation: Lymphocytes failed to organise into productive immune niches.
- Immunosuppressive myeloid niche: The density of M2-polarised macrophages increased, likely damping cytotoxic activity.
- Adaptive PD-1 up-shift: Post-treatment T cells displayed higher PD-1 expression, suggesting re-engagement of the PD-1/PD-L1 axis and a mechanism of resistance to avelumab.
Read the full paper
- Over the past two years, Cure51 has collected tumor samples from 1000 exceptional cancer survivors in collaboration with 100+ leading cancer centers worldwide.
- A first batch of tumor samples, processed and qualified at Institut Gustave Roussy in Paris, is being transferred in June 2025 to Explicyte—a Bordeaux-based CRO dedicated to precision oncology with unique capacities in single-cell spatial transcriptomics in Europe
PARIS, FRANCE, 26 June, 2025 - French TechBio startup company Cure51 set to unlock the biological mechanisms from cancer survivors, and precision oncology CRO Explicyte announced today a strategic partnership to analyze tumor samples from exceptional cancer survivors using single-cell spatial transcriptomic technologies. The resulting gene expression maps, generated at single-cell resolution, will be analyzed by Cure51’s data science team to uncover the molecular drivers of long-term survival and identify new therapeutic strategies.
Launched in November 2023, the Cure51’s Rosalind study seeks to decode the biological mechanisms of super responders—patients who defy the odds by surviving highly aggressive cancers—in collaboration with leading cancer centers around the world. The study targets three aggressive cancer types, Small Cell Lung Cancer (led by Charité, Berlin, Germany), Glioblastoma (led by Leon Berard, Lyon, France), and Metastatic pancreatic cancer (led by Gustave Roussy, Paris, France).
Cure51 has built a unique global network, partnering with 100 cancer centers to collect tumor samples and clinical data from over 1.000 cancer patients from 40 countries. The company’s mission is to create an unparalleled multi-omics database to drive the development of novel cancer therapies.
Leveraging Explicyte´s expertise in precision oncology and capitalizing on their deep experience of 10x genomics spatial tools and technology, Cure51 intends to accelerate its discovery process by better understanding the biology of Exceptional Survivors.
"At Cure51, we are reverse engineering the cure for cancer. By leveraging technology, data and our dedicated team of computational biologists, we aim to uncover the hidden biology of miraculous survivors, to develop therapies that could one day make cancer a manageable disease for all, “ said Cure51 co-Founders Nicolas Wolikow and Simon Istolainen. “ In just 18 months, our team forged international partnerships to secure access to tumor samples and clinical data from Cancer Outliers. To advance our data generation pipeline, we were looking for an EU-based partner with the scientific rigor and technical capabilities to process these valuable samples efficiently and reproducibly. Explicyte stood out for their strong scientific track record and cutting-edge technological expertise.”
"Over the past five years, first-generation spatial transcriptomics technologies have driven major advances in our understanding of the determinants of immunotherapy response, leading to over 30 co-authored publications with our academic and industry partners. In 2024, we took a significant step forward by establishing a unique single-cell spatial transcriptomics platform in Europe, built on 10x Genomics technologies. Cure51’s outlier-focused cohort is truly one of a kind. We are confident that this collaboration will generate transformative insights in the fight against cancer, and are excited to see Cure51 roll out."
— Alban Bessède, CEO, Explicyte
Earlier this year, Cure51 announced a major partnership with the Hopitaux de Paris (AP-HP), a network of 39 hospitals across France. In March 2024, the company raised €15 million in Seed funding led by Sofinnova Partners, Hitachi Ventures and LifeX. Cure51 is named after the British biochemist Rosalind Franklin, one of the greatest pioneers in medical research. Franklin and her doctoral student Ray Gosling captured the so-called ‘Photo 51’, which enabled the discovery of the double helix structure of DNA in 1953. The company’s motto is Cancer Delenda Est (Cancer is defeated).
About Cure51
Cure51 is a French techbio company founded by Nicolas Wolikow and Simon Istolainen alongside seasoned entrepreneurs and five world-renowned oncology centres: Gustave Roussy Cancer Campus (IGR, Paris - France), Leon Bérard Center (CLB, Lyon - France), Charité Universitätsmedizin Berlin (Germany), and Vall d'Hebron (VHIO, Barcelona, Spain). The collaboration between the private and public sectors is at the core of the Cure51 project, led by a passionate team with expertise in computing, medicine, and biology, and partnered with principal investigators across its network of over 50 leading oncology centres worldwide.
Cure51's exclusive data collection system, based on partnerships, enables the creation of a unique multimodal and multiomics database of Outliers. Using its discovery platform powered by computational modeling, Cure51 aims to understand the biological mechanisms responsible for this exceptional survival by identifying and validating targets that can act on these interactions, leading to first-in-class treatments. This research involves the use of all relevant models (in silico, in vitro, in vivo, ex vivo) and the integration of existing literature and available databases, along with the engagement of Cure51's KOL community. Ultimately, drug design will be subject to collaboration contracts with the industry.
For further information, please visit www.cure51.com
About Explicyte
Explicyte is a preclinical and translational contract research organization specializing in precision oncology. Founded in 2015 by immunologist Dr. Alban Bessède, the company has supported more than 100 biotech and pharmaceutical partners over the past decade in the discovery and development of novel therapies for solid tumors. Based at the Institut Bergonié Comprehensive Cancer Center in Bordeaux, Explicyte brings together a multidisciplinary team of 25 scientists, including cell biologists, digital pathologists, medical oncologists, and data scientists. In the past five years, Explicyte has co-authored over 30 peer-reviewed publications on the molecular mechanisms underlying responses to cancer immunotherapies.
For more information, visit www.explicyte.com
Press contacts
Cure51 – Clara Armand-Delille clara@thirdeyemedia.press
Explicyte – Pierre-Emmanuel GAULTIER - pe.gaultier@explicyte.com - +33 6 450 600 49
Download press kit (photos, bios, etc...)
Explicyte will attend the ASCO Annual Meeting in Chicago this June 2025.
Our CEO, Dr. Alban Bessède, will present two posters highlighting translational studies conducted in collaboration with leading academic and industry partners:
Alban will be available for 1:1 meetings during the event (June 1–3) to explore opportunities for collaborations in preclinical and translational research in precision oncology.
Our CEO, Dr. Alban Bessède, will present two posters highlighting translational studies conducted in collaboration with leading academic and industry partners:
- Spatial transcriptomics reveal crucial determinants of immune exclusion in non-small cell lung cancer From the Precision Medicine BIP Study In collaboration with GSK, Institut Bergonié, and Gustave Roussy
- CCR8⁺ regulatory T cells and their correlation with immunotherapy response in advanced NSCLC In collaboration with Bayer AG, Institut Bergonié, and Gustave Roussy
Alban will be available for 1:1 meetings during the event (June 1–3) to explore opportunities for collaborations in preclinical and translational research in precision oncology.
Book a 1:1 meeting
In a groundbreaking study led by Prof. Antoine Italiano from the Bergonié & Gustave Roussy Comprehensive Cancer Centers, 42 patients with advanced gastroenteropancreatic neuroendocrine neoplasms were treated with a combination of anti-PD-1/PD-L1 immunotherapy and the angiogenesis inhibitor regorafenib. The combination therapy resulted in increased response rates and improved survival outcomes compared to PD-1/PD-L1 immunotherapy alone. However, a significant portion of patients did not respond to this therapeutic regimen.
To uncover the mechanisms of resistance and identify potential predictive biomarkers, Explicyte developed a custom immunohistofluorescence (IHF) panel. Digital pathology revealed an overall increase in CD8+ T cell infiltration. In tumors from non-responding patients, we observed a higher proportion of PD1+ / IDO1+ neoplastic cells, suggesting the presence of an immunosuppressive environment mediated by tryptophan metabolism along the kynurenine pathway. This hypothesis was further supported by quantifying the Kynurenine/Tryptophan ratio, which was associated with IDO1 expression in tumor tissues and correlated with poorer clinical outcomes. Additionally, using Olink’s immuno-oncology and inflammation panels, we identified an enrichment of immune related proteins in the plasma of patients with high IDO1 activity. Soluble PD-L1, TNF receptor family members (OX40, CD40, 4-1BB), and the immunosuppressive cytokine interleukin-10 were associated with unfavorable outcomes.
Altogether, this translational study suggests shows that the combination of regorafenib plus avelumab is interesting for patients with highly pre-treated GEP NETs, and suggests that adding IDO1 inhibitors to the combination of anti-PD1/PDL1 therapy and anti-angiogenic agents could be a promising strategy to enhance patient responses.
To uncover the mechanisms of resistance and identify potential predictive biomarkers, Explicyte developed a custom immunohistofluorescence (IHF) panel. Digital pathology revealed an overall increase in CD8+ T cell infiltration. In tumors from non-responding patients, we observed a higher proportion of PD1+ / IDO1+ neoplastic cells, suggesting the presence of an immunosuppressive environment mediated by tryptophan metabolism along the kynurenine pathway. This hypothesis was further supported by quantifying the Kynurenine/Tryptophan ratio, which was associated with IDO1 expression in tumor tissues and correlated with poorer clinical outcomes. Additionally, using Olink’s immuno-oncology and inflammation panels, we identified an enrichment of immune related proteins in the plasma of patients with high IDO1 activity. Soluble PD-L1, TNF receptor family members (OX40, CD40, 4-1BB), and the immunosuppressive cytokine interleukin-10 were associated with unfavorable outcomes.
Altogether, this translational study suggests shows that the combination of regorafenib plus avelumab is interesting for patients with highly pre-treated GEP NETs, and suggests that adding IDO1 inhibitors to the combination of anti-PD1/PDL1 therapy and anti-angiogenic agents could be a promising strategy to enhance patient responses.
Read article in Nature Cancer
Alban Bessede, CEO of Explicyte, will attend the Meet2win oncology event in Bordeaux, France (May 6-7).
He will be available for 1:1 meetings over this 2-day event, to discuss potential preclinical and translational research opportunities.
He will be available for 1:1 meetings over this 2-day event, to discuss potential preclinical and translational research opportunities.
Alban Bessede, CEO, and Jean-Philippe Guegan, CTO, will present 2 posters at the 2025 AACR annual meeting in Chicago (April 25-30):
Feel free to reach out to them to arrange an on-site meeting!
- Impact of Immune Contexture on Immunotherapy Response in NSCLC: Insights from Multiplex IHC and Machine Learning-Based Phenotyping
- Tertiary Lymphoid Structures as Predictors of Immune Checkpoint Inhibitor Efficacy in NSCLC and the Development of an Ex Vivo Model for Precision Medicine
Feel free to reach out to them to arrange an on-site meeting!
Book a 1:1 meeting
Join us for an insightful session on March 27th, featuring the first authors behind three influential 2025 papers on tertiary lymphoid structures (TLS) in cancer:
Presenting a groundbreaking 2025 Nature paper, "IL-33-activated ILC2s induce tertiary lymphoid structures in pancreatic cancer". Dr. Amisaki’s work deepens our understanding of TLS biology and paves the way for innovative therapeutic strategies for transforming “cold” tumors into immunologically active environments.
Sharing findings from his PhD research, conducted at Explicyte, Dr. Peyaud will discuss 2 publications:
Immunologist Alban Bessede, PhD, CEO of Explicyte, will kick off the session. Dr Bessede has been working on TLS since 2020, co-authoring foundational papers in Nature Cancer and Nature Medicine on TLS & immune-checkpoint inhibitors, and is now developing accredited pathology services for detecting and scoring TLS in tumor specimens to support precision oncology initiatives.
Masataka Amisaki, MD, PhD, MSKCC (USA)
Presenting a groundbreaking 2025 Nature paper, "IL-33-activated ILC2s induce tertiary lymphoid structures in pancreatic cancer". Dr. Amisaki’s work deepens our understanding of TLS biology and paves the way for innovative therapeutic strategies for transforming “cold” tumors into immunologically active environments.
Florent Peyraud, MD, PhD, Institut Bergonié (France)
Sharing findings from his PhD research, conducted at Explicyte, Dr. Peyaud will discuss 2 publications:
- A research paper in Cell Reports Medicine titled "Spatially resolved transcriptomics reveal the determinants of primary resistance to immunotherapy in NSCLC with mature tertiary lymphoid structures"
- A comprehensive review in Med. titled "Tertiary lymphoid structures and cancer immunotherapy: From bench to bedside"
Session Introduction
Immunologist Alban Bessede, PhD, CEO of Explicyte, will kick off the session. Dr Bessede has been working on TLS since 2020, co-authoring foundational papers in Nature Cancer and Nature Medicine on TLS & immune-checkpoint inhibitors, and is now developing accredited pathology services for detecting and scoring TLS in tumor specimens to support precision oncology initiatives.
Register for the webinar
This translational research paper highlights the work of Florent Peyraud, MD, conducted during his PhD thesis at Explicyte under the supervision of Prof. Antoine Italiano (Bergonié & Gustave Roussy Comprehensive Cancer Centers) and Alban Bessede, PhD (Explicyte). This project was made possible thanks to a collaboration with the imCORE network (Roche/Genentech), and samples from the BIP trial (NCT02534649). The study aims to uncover why certain patients with non-small cell lung cancer (NSCLC) who exhibit mature tertiary lymphoid structures (mTLS)—a phenotype typically associated with a favorable response to immune checkpoint inhibitors (ICI)—do not respond to anti-PD1/PD-L1 immunotherapy.
Presence of mature TLS & clinical outcome in NSCLC
A comprehensive pathological analysis of 509 NSCLC patients treated with immune checkpoint inhibitors (ICI) was performed, confirming that the presence of mTLS predicts a better outcome in terms of response rate, overall survival, and median progression-free survival, independently of PD-L1 and genomic features.
Spatial transcriptomics in responding & non-responding mTLS-positive NSCLC patients
Specimens from 6 mTLS-positive patients with extreme ICI response (3 responders, 3 non-responders) were analyzed using the GeoMx Whole Transcriptome Atlas. While gene expression profiles did not differ within the TLS and tumor compartments, non-responders exhibited an enrichment in fibroblasts in the stromal compartment, with a pronounced expression of TGFβ signaling and epithelial-mesenchymal transition (EMT) pathways.
Multiplex immunohistofluorescence (mIHF) panel focusing on cancer-associated fibroblasts (CAFs) 77 m-TLS positive patient samples were then analyzed by digital pathology for the detection of tumor cells, cytotoxic CD8+ T cells, and FAP+αSMA+ CAF and MYH11+αSMA+ CAFs. Analysis revealed a higher stromal density of both CAF subsets in non-responders, correlating with poor clinical outcome.
Bulk transcriptomics to analyze interactions between the immune infiltrates & CAF status
Gene expression profiling of 40 mTLS-positive lung tumor samples identified that:
Multiplex immunofluorescence panel focused on T cell exhaustion
Specimens of 64 mTLS positive NSCLC patients were then analyzed by digital pathology:
Altogether, these findings suggest that the presence of FAP+αSMA+ CAFs and MYH11+αSMA+ CAFs is associated with poor outcomes in mTLS-positive NSCLC patients undergoing ICI treatment. They could serve as biomarkers to stratify patients, and could constitute targets, in combination with strategies addressing T-cell exhaustion, to enhance ICI efficacy in mTLS-positive NSCLC patients.
Interested in the assessment of TLS maturity? Learn about our histopathology services for TLS detection & scoring.
Presence of mature TLS & clinical outcome in NSCLC
A comprehensive pathological analysis of 509 NSCLC patients treated with immune checkpoint inhibitors (ICI) was performed, confirming that the presence of mTLS predicts a better outcome in terms of response rate, overall survival, and median progression-free survival, independently of PD-L1 and genomic features.
Spatial transcriptomics in responding & non-responding mTLS-positive NSCLC patients
Specimens from 6 mTLS-positive patients with extreme ICI response (3 responders, 3 non-responders) were analyzed using the GeoMx Whole Transcriptome Atlas. While gene expression profiles did not differ within the TLS and tumor compartments, non-responders exhibited an enrichment in fibroblasts in the stromal compartment, with a pronounced expression of TGFβ signaling and epithelial-mesenchymal transition (EMT) pathways.
Multiplex immunohistofluorescence (mIHF) panel focusing on cancer-associated fibroblasts (CAFs) 77 m-TLS positive patient samples were then analyzed by digital pathology for the detection of tumor cells, cytotoxic CD8+ T cells, and FAP+αSMA+ CAF and MYH11+αSMA+ CAFs. Analysis revealed a higher stromal density of both CAF subsets in non-responders, correlating with poor clinical outcome.
Bulk transcriptomics to analyze interactions between the immune infiltrates & CAF status
Gene expression profiling of 40 mTLS-positive lung tumor samples identified that:
- FAP+αSMA+ CAF-High tumors were associated with inflammatory response and T-cell exhaustion, which may explain the limited efficacy of ICI.
- MYH11+αSMA+ CAF-High tumors were associated with an enrichment in regulatory T cell (Treg) gene signatures, which are known to participate in immunosuppression and be detrimental to ICI efficacy
Multiplex immunofluorescence panel focused on T cell exhaustion
Specimens of 64 mTLS positive NSCLC patients were then analyzed by digital pathology:
- A panel consisting of CD8, PD1, CD39, LAG3, TIGIT, TIM3, and DAPI revealed a high density of intratumoral CD8+PD1+ T cells in the FAP+αSMA+ CAF-High tumors, with a higher expression of exhaustion markers.
- A panel including CD4, CD8, CD20, FoxP3, ICOS, TIGIT and DAPI highlighted an increased presence of CD4+ T cells in the stroma of MYH11+αSMA+ CAF-High tumors, with an increased infiltration of regulatory CD4+FoxP3+ T cells expressing immunosuppressive markers.
Altogether, these findings suggest that the presence of FAP+αSMA+ CAFs and MYH11+αSMA+ CAFs is associated with poor outcomes in mTLS-positive NSCLC patients undergoing ICI treatment. They could serve as biomarkers to stratify patients, and could constitute targets, in combination with strategies addressing T-cell exhaustion, to enhance ICI efficacy in mTLS-positive NSCLC patients.
Interested in the assessment of TLS maturity? Learn about our histopathology services for TLS detection & scoring.
Read paper
Over the past 5 years, Explicyte has supported several cancer immunotherapy programs aimed at inducing or enhancing a specific anti-tumor immune response. Here's a quick overview of our capacities for the advancement of novel cancer vaccines (peptide-based, DC-based, DNA- or RNA-based), cytokine therapies, oncolytic virus-based therapies, immune modulators (such as STING agonists), and immune adjuvants.
We designed a cell-based system to assess the effectiveness of compounds aimed at enhancing the proficiency of antigen-presenting cells (APC), such as dendritic cells (DC), to capture and cross-present the tumor antigens, and the subsequent priming of CD8+ cytotoxic T cells against cancer cells. The assay provides dynamic flexibility, thus fitting different typologies of test compounds, with different modes of action and treatment modalities.
CASE STUDY
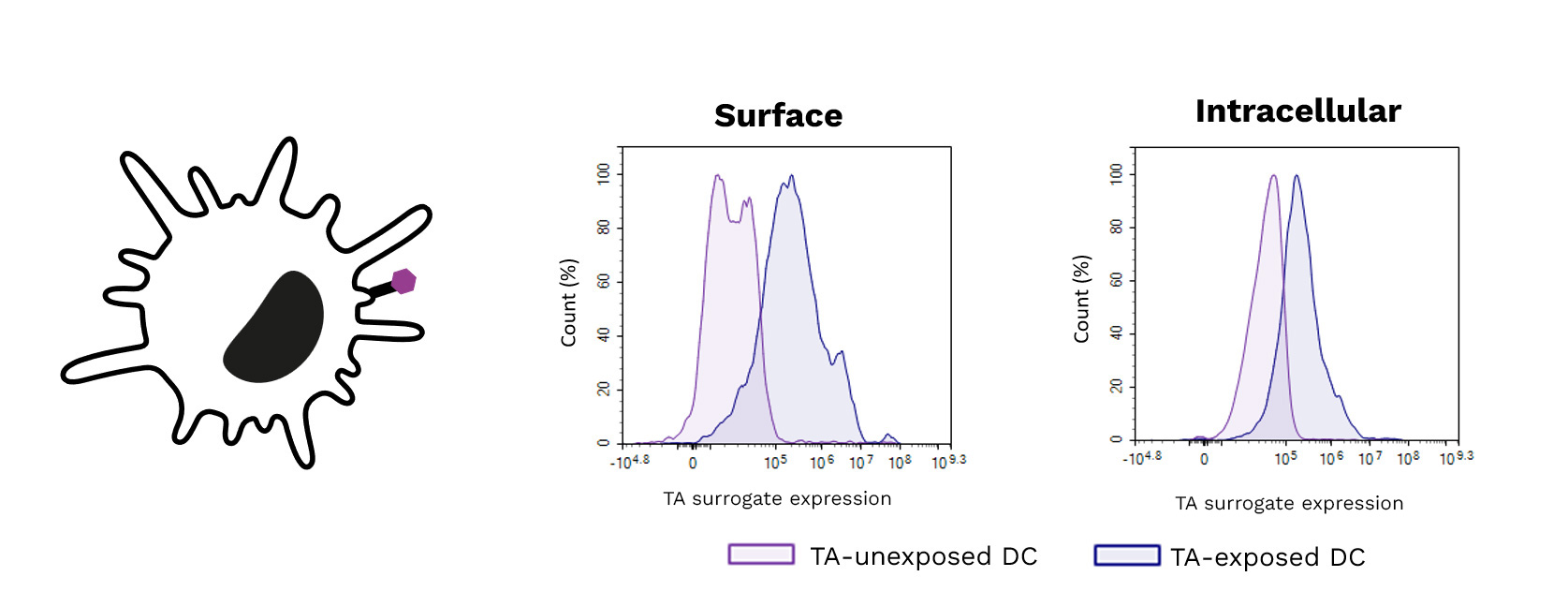
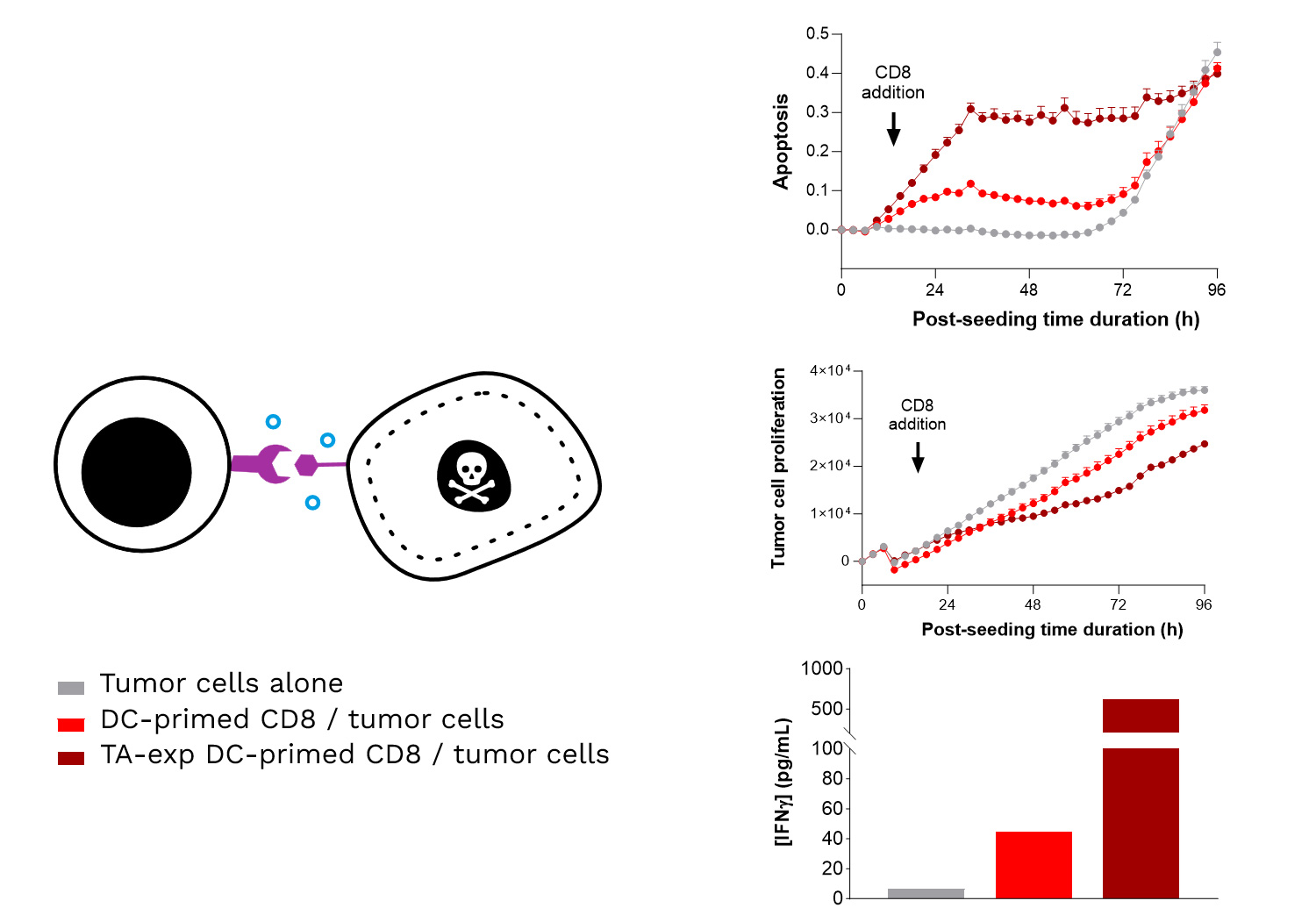
Exposure of DCs to a target tumor antigen (TA) peptide enhances their antigenic presentation shown by the increase of its surrogate expression (surface (left) and intracellular (right)) using specific antibodies.
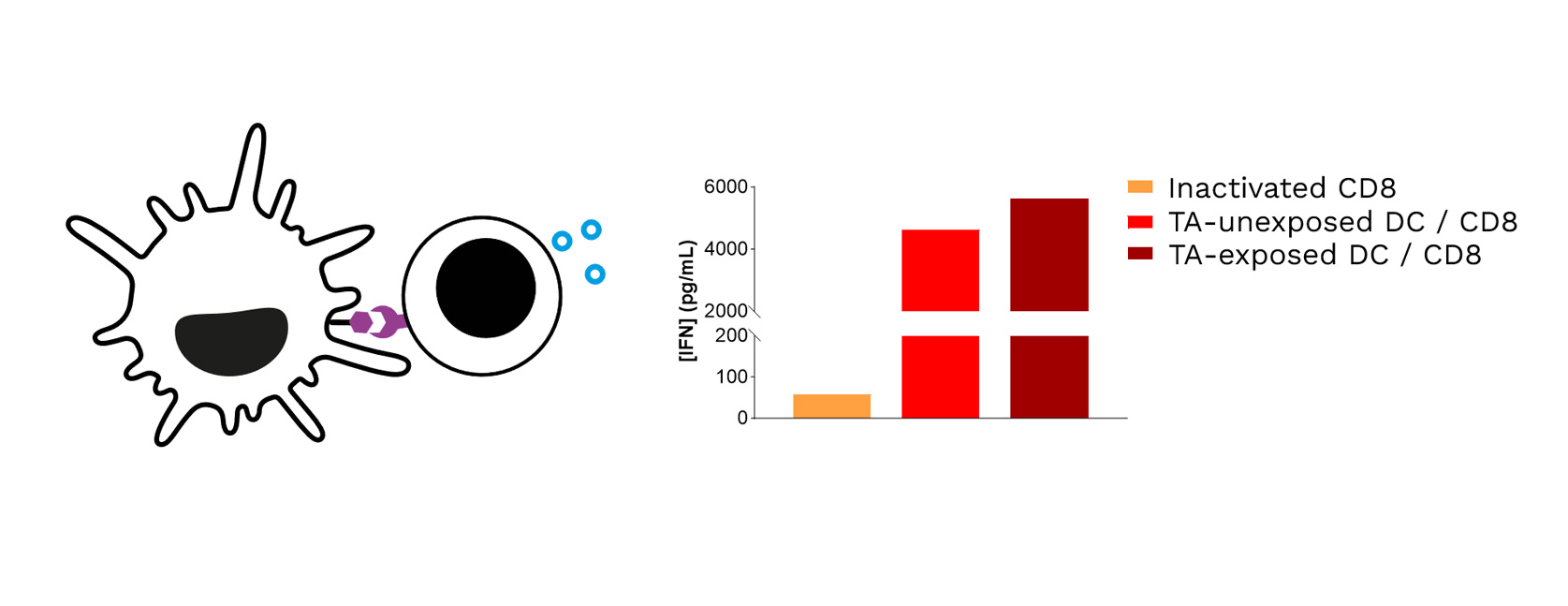
Target TA-exposed DCs lead to optimized priming of CD8 T cells, as shown through the increased IFNγ levels released in CD8 T cell / DC co-cultures.
Specific TA-exposed DC-mediated priming of CD8 T cells results in the induction of an adaptive effector T cell-mediated killing towards SK-MEL-5 tumor cells (target TA-positive). Real-time monitoring of SK-MEL-5 tumor cell killing mediated by CD8 T cells, primed by either TA-exposed or unexposed DCs, where apoptosis and tumor cell count were monitored over ~4 days and analyzed. In addition, IFNγ release by CD8 T cells is shown to be increased upon their TA-exposed DC priming, compared to TA-unexposed DCs.
TAKE HOME MESSAGE: Enhancing DC-mediated tumor antigen presentation induces a specific, optimized, adaptive effector T cell-mediated killing response.
A step-by-step overview of our tumor antigen-specific T-cell mediated tumor killing assay:
Starting from FFPE tumor specimens, our translational team can explore and/or validate the expression of target tumor antigens across a set of cancer indications, using various platforms:
Talk to a scientist from our translational team
Specific Tumor Antigen Presentation: In vitro Efficacy & MoA Studies with a dedicated DC-mediated T-cell Killing Assay
We designed a cell-based system to assess the effectiveness of compounds aimed at enhancing the proficiency of antigen-presenting cells (APC), such as dendritic cells (DC), to capture and cross-present the tumor antigens, and the subsequent priming of CD8+ cytotoxic T cells against cancer cells. The assay provides dynamic flexibility, thus fitting different typologies of test compounds, with different modes of action and treatment modalities.
CASE STUDY
Exposure of DCs to a target tumor antigen (TA) peptide enhances their antigenic presentation shown by the increase of its surrogate expression (surface (left) and intracellular (right)) using specific antibodies.
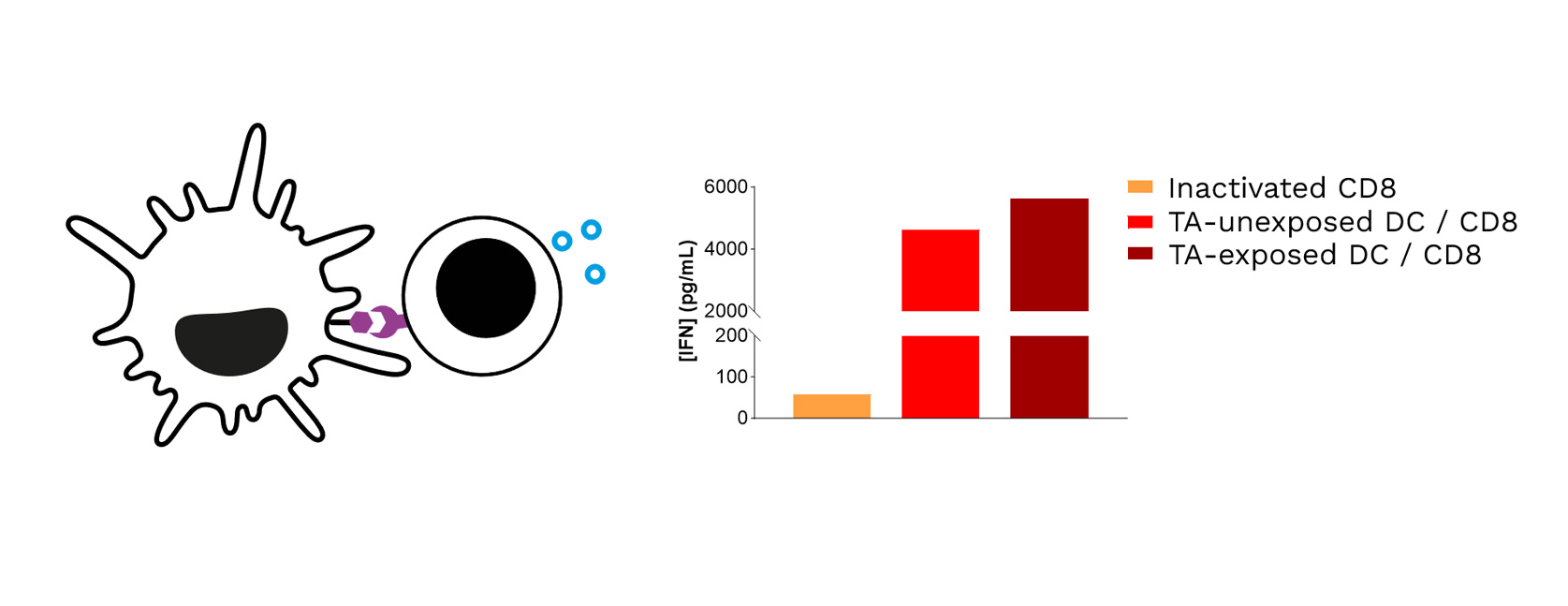
Target TA-exposed DCs lead to optimized priming of CD8 T cells, as shown through the increased IFNγ levels released in CD8 T cell / DC co-cultures.
Specific TA-exposed DC-mediated priming of CD8 T cells results in the induction of an adaptive effector T cell-mediated killing towards SK-MEL-5 tumor cells (target TA-positive). Real-time monitoring of SK-MEL-5 tumor cell killing mediated by CD8 T cells, primed by either TA-exposed or unexposed DCs, where apoptosis and tumor cell count were monitored over ~4 days and analyzed. In addition, IFNγ release by CD8 T cells is shown to be increased upon their TA-exposed DC priming, compared to TA-unexposed DCs.
TAKE HOME MESSAGE: Enhancing DC-mediated tumor antigen presentation induces a specific, optimized, adaptive effector T cell-mediated killing response.
How does it work?
A step-by-step overview of our tumor antigen-specific T-cell mediated tumor killing assay:
- Choice of the right tumor cell lines based on their expression of the target antigens and their representativeness of the cancer indications of interest (>100 in-house human tumor cell lines)
- Isolation of PBMC-originating immune populations required (monocytes, CD8) for autologous co-cultures
- Generation of monocyte-derived APC such as differentiated & mature DCs
- DC - CD8 T cell co-cultures for DC-mediated priming and activation of CD8 cells
- CD8 T cell - target tumor cell co-cultures to capture the tumor-targeted cytotoxic response
- Adequate treatment windows in line with the expected mechanisms of action and eventual promising combination treatments that could hold potential for improving anti-tumor response
- Relevant readouts to capture each cell component (DC cytokines and surface markers, CD8 cytokines and surface markers, target tumor cell apoptosis/proliferation…)
More data ? Some questions ? Contact our team !
Our capacities for the identification & Validation of Target Antigen Expression in Tumor Samples
Starting from FFPE tumor specimens, our translational team can explore and/or validate the expression of target tumor antigens across a set of cancer indications, using various platforms:
- Single-Cell RNA-Seq to identify & quantify tumor antigen expression, and investigate tumor antigen heterogeneity and the immune landscape
- Xenium Single-Cell Transcriptomics to explore tumor antigen patterns and tumor heterogeneity with respect to the immune microenvironment (immune infiltration, response, gene expression profiles and signatures…)
- GeoMx Digital Spatial Profiling for comprehensive antigen mapping within the tumor microenvironment (TME)
- Digital Pathology for precise and multiplexed analysis of antigen expression with the TME - providing a comprehensive view of the tumor antigenic profile and how it could interact with other components of the TME
Talk to a scientist from our translational team